Leaving well: The 2023 Action Plan for Successful Ageing
Raising awareness of end-of-life care and pre-planning as well as smoothing discharge processes from hospitals and encouraging earlier referrals to palliative care are two of the four main measures announced as part of an updated national blueprint on Jan 30.
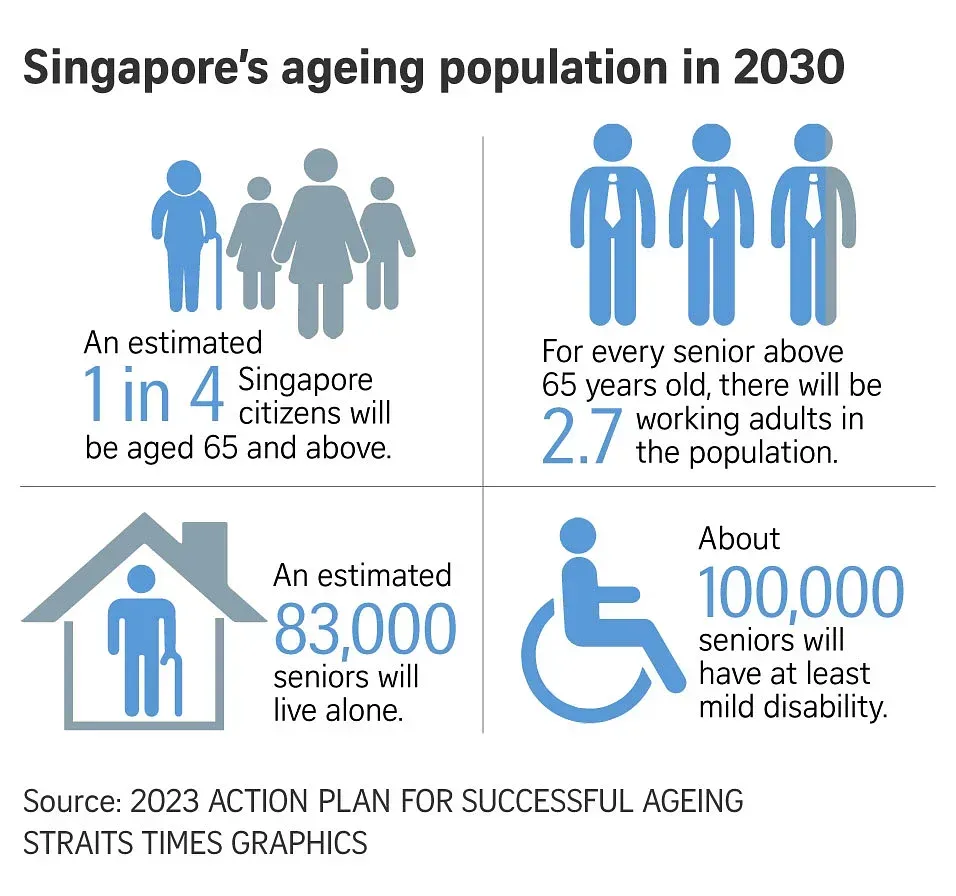
The 2023 Action Plan for Successful Ageing (download it here) is an extension of the 2015 Action Plan for Successful Ageing.
In the former, the following guidelines and measures to enhance the capacity, affordability and quality of palliative care to support an ageing population were laid out:
- MOH will increase the number of inpatient palliative care beds from 182 to 360 by 2020, and serve 1,000 more home palliative care patients.
- The Singapore Hospice Council will promote and implement a set of National Guidelines for Palliative Care.
- MOH has raised the Medisave withdrawal limits for both inpatient and home-based palliative care, and lifted Medisave withdrawal limits for home-based patients with cancer or end-stage organ failure.
- MOH has improved funding for home palliative care providers by moving away from funding based on the number of visits made to patients to funding based on a fixed amount for every patient under their care each month.
- MOH is also in the midst of rolling out subsidies for day hospice services, which brings together social and healthcare services for patients under palliative care.
Enhancing Singaporeans’ knowledge of palliative and end-of-life care
Since 2015, major strides have been made in improving access to palliative care for Singaporeans. As early as January 2015, the Singapore Hospice Council had formulated the inaugural edition of the National Guidelines for Palliative Care, thereby fulfilling one of the strategies laid out in the 2011 report on the National Strategy for Palliative Care developed by the Lien Centre for Palliative Care.
The Singapore Hospice Council is also developing a training framework on palliative care, a step deemed necessary by MP Yip Hon Weng (Yio Chu Kang) during the 2022 debate on the budget statement. The steps taken since, 2018, to enhance the enhance the knowledge and understanding of palliative and end-of-life care amongst healthcare professionals include:
- The National Outcomes Framework for Medical Graduates that guides medical schools in developing their curricula and specifies core learning outcomes on palliative car was introduced in December 2018.
- Local nursing schools provide palliative care training to all nurses.
- The Palliative Nursing Competency Framework was rolled out in October 2022.
- The Singapore Hospice Council and the Agency for Integrated Care have been increasing awareness of palliative care and end-of-life issues amongst healthcare professionals through regular training courses, seminars and conferences.
As of end November 2022, over 100 physicians had undergone the Graduate Diploma in Palliative Medicine programme.

Care for palliative and end-of-life patients and their caregivers
The 2015 Action Plan had aimed to increase the number of palliative care beds from 182 to 360 by 2020. In a October 2021 reply to a written question by MP Joan Pereira (Henderson-Dawson), Health Minister Ong Ye Kung stated that there are currently a total of 255 inpatient beds for palliative care, of which 155 are in hospices and the remaining 100 in community hospitals, with occupancy rate being “close to 70% over the past year”.
In the same reply, Mr Ong also reiterated the governments commitment to “continue to ensure sufficient inpatient and home palliative care capacity to meet the future needs of our population”.
Further, to reduce the risk of caregivers burn-out, MOH has since 2019 implemented a Home-Based Respite Care pilot, as part of the 2018 Care-giver Support Action Plan, to allow caregivers some rest while a trained caregiver steps in temporarily to care for their loved ones.
The Home-based respite care pilot for palliative cancer patients that was introduced in in September 2019 and expanded to all patients receiving home palliative care, regardless of diagnosis, in 2021.
Read more: Speech by Mr Ong Ye Kung, Minister for Health, At the 7th Singapore Palliative Care Conference
Paying for palliative and end-of-life care
Since 2015, for patients who are diagnosed with terminal cancer and receiving end-of-life care, MediSave may be used to pay for home palliative care or day hospice care, and there is no withdrawal limit if the bill is paid using the patient’s own MediSave.
In addition, patients with financial needs can apply for MediFund assistance, which helps to provide a safety net for those who are still unable to afford the bills.
A CPF member may use up to $250 (general) or $350 (specialised) per day from his/her MediSave for approved inpatient hospice palliative care services (IHPCS).
The combined lifetime withdrawal limit for day hospice and home palliative care is $2,500 per patient, but there will not be any limit if you’re diagnosed with terminal cancer or end-stage organ failure.
The above measures to enhance palliative and end of life care are, as of December 2021, encapsulated in MOH’s National Strategy for palliative care, in particular these three areas: (i) supporting caregivers, (ii) expanding palliative care capacity and (iii) raising palliative care capability.

Photo: The Straits Times
The 2023 Action Plan for Successful Ageing
Thus, the measures, as laid out in the 2023 Action Plan for Successful Ageing, that focuses on preparing for end-of-life in a rapidly ageing Singapore, should thus be view as a continuation of government policies the and good work done by the respective stakeholders, including but notwithstanding Singapore Hospice Council, hospices, hospitals and local arts group.
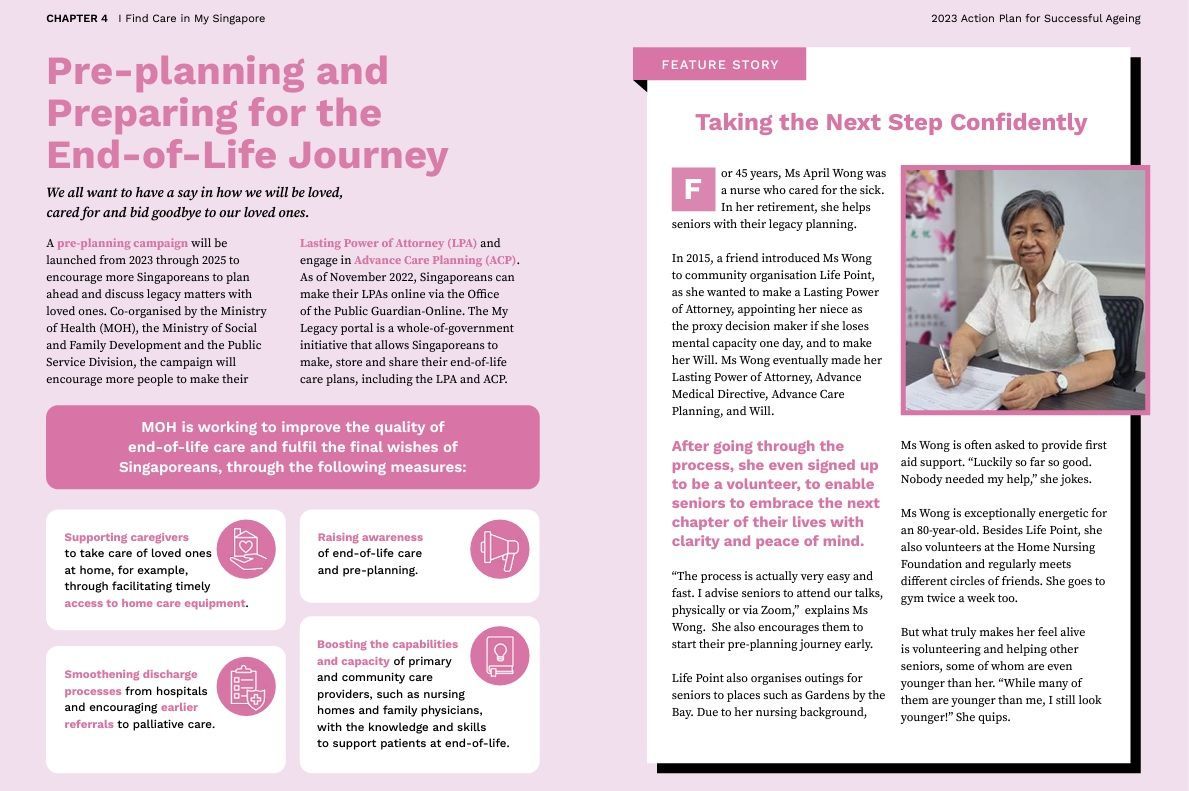
MOH will improve the end-of-life care and fulfil the final wishes of Singaporeans, through the following measures:
- Supporting caregivers to take care of loved ones at home
- Raising awareness of end-of-life care and pre-planning.
- Smoothening discharge processes from hospitals and encouraging earlier referrals to palliative care
- Boosting the capabilities and capacity of primary and community care providers, such as nursing homes and family physicians, with the knowledge and skills to support patients at end-of-life.
In fact, these measures should not come as a surprise as they were highlighted by Health Minister Ong in a parliamentary reply to a written question by MP Yip in October 2022.
To this end, a pre-planning campaign will be launched from 2023 through 2025 to encourage more Singaporeans to plan ahead and discuss legacy matters with loved ones, including the drafting Lasting Power of Attorneys (LPA) and engage in Advance Care Planning (ACP) - as of November 2022, Singaporeans can make their LPAs online via the Office of the Public Guardian-Online.
It is hoped with these efforts will help to reduce proportion of deaths in hospitals from 61 per cent to 51 per cent by 2027. It is also hoped that by the end of 2025, more than 24,000 Singaporeans aged 50 and above will register for LPA, according to CNA.
As of June 2022, a total of 152,000 people has registered their Lasting Power of Attorney (LPA) – however, the percentage of our population above 60 years old by 10-year bands on their adoption of LPA is not publicly known.
Source: The 2023 Action Plan for Successful Ageing


